Beyond Biology: Racial Disparities in Prostate Cancer and Their Mental Health Toll
How does prostate cancer impact men differently across racial and ethnic groups, with African-American men facing the heaviest burden? Beyond biology, systemic inequities and socioeconomic barriers fuel profound psychological distress for patients and families. Discover how targeted screening, equitable care, and mental health support could transform outcomes—and why ignoring this human side deepens the crisis.
Mercy Nwankama, PMHNP-BC, MSN
9/22/20242 min read
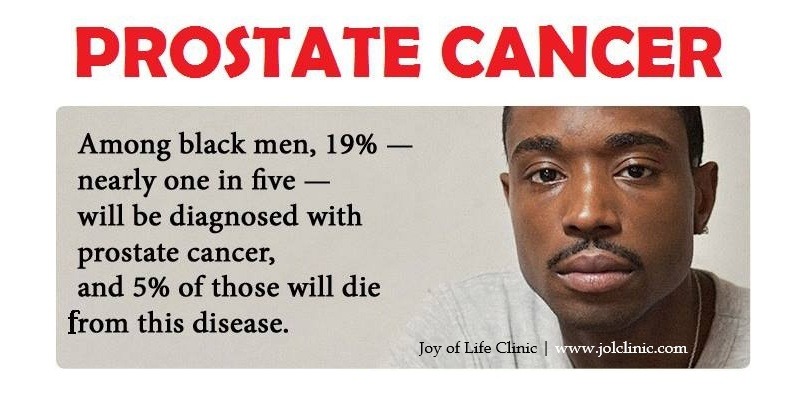
The article by Nobuyuki Hinata, and Masato Fujisawa, titled Racial Differences in Prostate Cancer Characteristics and Cancer-Specific Mortality: An Overview caught my attention. The authors reviewed how prostate cancer disproportionately affects men of different racial and ethnic backgrounds, with African-American men facing higher incidence, earlier onset, and worse survival outcomes compared to Caucasian men, and with rising incidence in parts of Asia.
While the piece focuses on biology, I believe that socioeconomic status, and access to care, these disparities carry profound psychological consequences. Patients from high-risk groups often live under heightened anxiety, facing not only the fear of the disease itself but also the stress of knowing their demographic history places them at greater risk. Families, in turn, may carry anticipatory grief, helplessness, and frustration when systemic inequities limit treatment options.
The article highlights that disparities stem from both genetic differences and structural inequalities in healthcare delivery. From a mental health perspective, this combination compounds distress: the perception of being biologically predisposed to poorer outcomes may foster fatalism, while socioeconomic barriers can erode hope and trust in medical systems.
Conversely, targeted screening, equitable access to care, and culturally sensitive education campaigns have the potential to ease this burden by giving patients and families a sense of agency and fairness. Thus, addressing prostate cancer disparities is not only a medical necessity but also a crucial component of reducing psychological trauma across affected communities.
Mental Health–focused Recommendations
For clinicians and policymakers, drawn from the article’s findings and reframed through the psychological impact lens:
For Clinicians
Integrate mental health screening into cancer care: Alongside PSA testing and clinical evaluations, routinely assess for anxiety, depression, and caregiver strain, especially in high-risk populations.
Provide culturally sensitive counseling: Acknowledge the historical and racial disparities that may amplify fear or mistrust. Validating these concerns can reduce alienation and build a therapeutic alliance.
Offer family-centered support: Since families often bear the weight of caregiving and anticipatory stress, extend education and psychological resources to spouses, children, and extended relatives.
Address fatalism proactively: When discussing genetic or racial risk factors, frame them in terms of empowerment (e.g., “this means earlier monitoring gives us more options”) rather than inevitability.
For Policymakers
Expand access to psychosocial services in cancer programs, particularly for underserved communities where disparities in incidence and mortality are greatest.
Fund community-based mental health education to normalize discussions of prostate cancer and reduce stigma in high-risk groups, lessening the isolation families often experience.
Support caregiver resources (respite programs, counseling subsidies, peer networks) to mitigate burnout and long-term emotional harm in families.
Incorporate mental health outcomes into cancer equity metrics, ensuring reforms are measured not just by survival rates but also by reductions in psychological distress.
In short, closing racial gaps in prostate cancer care requires not only better screening and treatment, but also systematic attention to the emotional well-being of patients and their families.
Reference
Hinata N, Fujisawa M. Racial Differences in Prostate Cancer Characteristics and Cancer-Specific Mortality: An Overview. World J Mens Health. 2022 Apr;40(2):217-227. doi: 10.5534/wjmh.210070. Epub 2022 Jan 1. PMID: 35021294; PMCID: PMC8987139.

Home | About Us | Our Services | Blog | Terms & Conditions | Privacy | Telehealth | Forms & Resources | Appointments | Log In | Site Map | Contact Us
BY APPOINTMENT ONLY | NO WALK-IN
BEST WAY TO CONTACT US
Sign In to your account or Fill out the Contact Form or Appointment Form
or
Send us an Email at admin@jolclinic.com
Tel: (410) 231-3118 | Fax: (410) 262-6911
PATIENT RECORDS
To request your patient records, please sign in or go to the patient records information page.
Copyright © 2024 by the Joy of Life Clinic LLC.
4900 Belair Road
Baltimore MD 21206